Diabetic foot infection requires special mention because of its peculiar characteristics, which make it different and difficult to treat. Patients with diabetes develop three types of conditions affecting their legs and feet, which are responsible for the intractable nature of foot infections in diabetic patients. Though these conditions evolve over a period of time, they certainly happen to a variable extent.
These are vasculopathy, neuropathy, and limited joint mobility. In short, vasculopathy is a condition causing narrowing of arteries of the legs and feet, leading to a gradual reduction in the blood supply to toes, feet and legs; neuropathy is a condition of having decreased sensations in the sole of the foot, making it impossible for the patient to perceive pain due to injury and infection; and limited joint mobility is the condition of decreased elasticity and plasticity of fascia, ligaments and joints of foot leading to abnormal weight bearing patterns and consequent ulcerations.
Collectively, all three conditions, along with very high/fluctuating blood sugar levels, can complicate a simple-looking infection or a minor injury of the foot in a diabetic patient into severe cellulitis or gangrene. And there comes the role of a plastic surgeon in treating these infections. By virtue of his/her extensive training in dealing with soft tissue infections, in-depth anatomical knowledge of all structures of foot, and ability to reconstruct the soft tissue defects, a plastic surgeon is the best doctor to deal with such resistant diabetic foot infections.
Diabetes itself is one of the most important risks for the development of infections. However, if diabetes is well controlled, the chances of foot infection diminish to a great extent. Lower limb arteries (blood vessels carrying blood from the heart to the toes) are commonly affected by atherosclerosis (decreased internal diameter due to the deposition of cholesterol crystals) in diabetic patients, and this decreased blood supply to the toes of the feet is another major cause of foot infection.
Neuropathy (decreased sensations) affecting the nerves of the foot is also a very important risk factor for the development of infection in a diabetic patient. Many incidences of infection in diabetic patients are preceded by history of some minor trauma or even friction by ill-fitting shoes. Initially, most of these infections present as cellulitis of the foot and leg leading to swelling, increased redness and tenderness of affected area. If unchecked at an early stage of cellulitis, infection in the foot of a diabetic patient can propagate very fast and can lead to disastrous consequences like gangrene and invasive systemic sepsis. In such unfortunate events, either patient loses his/her digits, limb or has to struggle a lot even to survive.
Management of a patient with diabetic foot infection requires team approach. Strict control of blood sugar levels, timely administration of antibiotics, very good general nursing care, absolute bed rest with proper elevation of affected limb, regular timely dressing changes and the most important is the decision to do surgery. Plastic surgeon as a leader of team managing diabetic foot infection is the best person to coordinate amongst team members and decide about the perfect timing and planning of surgical procedure. Many such diabetic foot infection patients require staged surgical approach and, in such complicated situations, importance of Plastic surgeon increases even more than usual.
Treatment of diabetic foot infection not only requires deep understanding of the anatomy of foot, but it requires thorough understanding of vasculopathy, neuropathy and limited joint mobility occurring in diabetic patients. Based on these understanding and consideration of all patient related factors supported by necessary investigations, plastic surgeon formulates the treatment plan for diabetic foot patient. Treatment is centred towards complete resolution of foot infection and healing of all the wounds. Apart from therapeutic angle, prevention of foot infection is also equally important.
For prevention to be effective, patient and his/her family members are counselled by treating plastic surgeon him/herself and importance of daily foot care is emphasized to them. For both treatment of existing foot ulcers and prevention of future ulcers in the foot, the latest and novel concept of “Internal Offloading Surgery” is the key. Plastic surgeon identifies the underlying cause of the ulcer by his clinical experience and acquired expertise. And by doing surgery to correct the problem (deformity) responsible for ulcer development, plastic surgeon serves the dual purpose for the patient; healing and prevention of foot ulcers.
At cutis hospital, all patients of diabetic foot infections are examined and treated by an experienced and expert plastic surgeon. We have a specialized, dedicated O.P.D. for patients of diabetic foot in which all patients of diabetic foot are examined by a team of Plastic surgeon, Interventional endovascular specialist and a Prosthesis specialist.
Thus, the best possible management plan is decided and explained to the patient. All patients of diabetic foot are counselled and educated about the importance and method of daily foot care. Podiatry services are also offered and a customized and very useful diabetic foot care kit is made available (on commercial basis) to the patients for home use.
Apart from this comprehensive diabetic foot O.P.D. at Cutis Hospital, there are facilities of state-of-the-art operation theatres, round the clock nursing staff and indoor facilities. Patients can choose between different category of rooms and stay as long as it is needed.






Any infection happening in the toes, heel, sole, or dorsum of the foot in a patient with diabetes is called a diabetic foot infection.
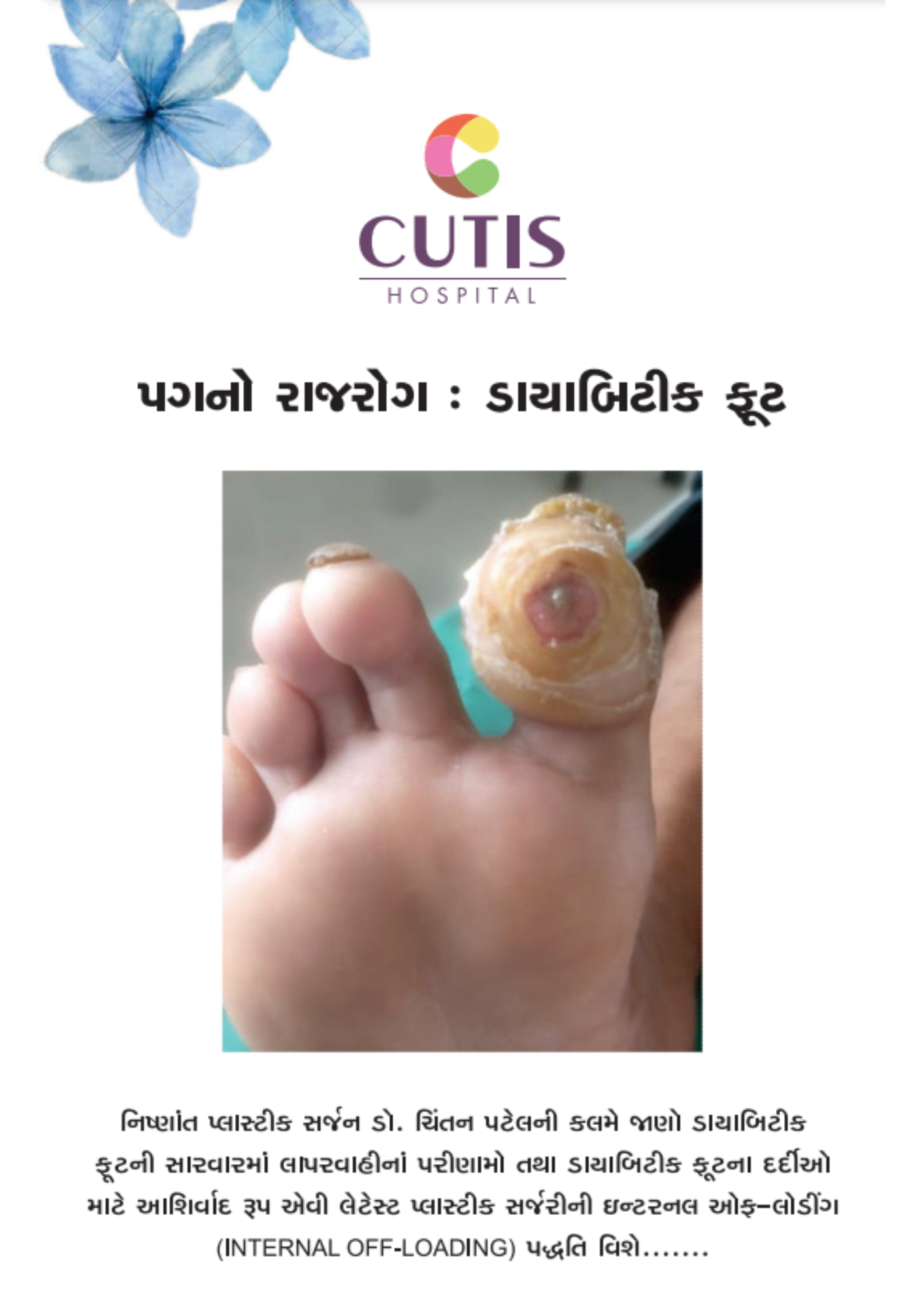
A diabetic foot infection usually starts with a callus. Callus is a localized thickening of the skin of the sole due to constant pressure and friction. Though callous formation is a protective mechanism of our body; if not addressed, constant pressure and friction gradually end in an ulcer developing beneath the callous, called a sub-callous ulcer.
This sub-callous ulcer is the culprit for the majority of deadly foot infections in diabetic patients. Apart from callous, minor injuries like thorn pricks, nail injury, and friction due to ill-fitting shoes are also the reasons for serious diabetic foot infections.
No. However, patients with foot infections with diabetes (diabetic foot patients) definitely have more chances of developing gangrene than similar patients with foot infections without diabetes.
Because patients with diabetes usually have neuropathy and vasculopathy. Due to neuropathy, these patients keep on walking over an ulcer of the sole, and they are not aware of the ongoing tissue trauma.
By the time the patient reaches a plastic surgeon, the infection has usually progressed to a significant level. Coupled with neuropathy, they do have vasculopathy. Vasculopathy reduces blood flow in the arteries of the lower limbs to a great extent in many diabetic patients. Due to very poor blood circulation in the toes and feet, even minor trauma or injury in such a compromised condition refuses to heal and can terminate in tissue death called gangrene.
No. Patients with diabetes have a foot infection with the same type of bacteria as other non-diabetic people. More than the type of bacteria causing infection, the conditions of the patient’s tissues are responsible for the seriousness of the infection.
A non-diabetic patient with normal sensations will complain of excruciating pain upon the development of even a small infection in his foot, forcing him/her to seek medical help and rest. Patients with diabetes keep on walking over the foot infection, which pushes the bacteria higher, leading to the advanced stage of infection by the time the patient approaches a doctor.
Many patients with diabetes have decreased blood supply to their feet and toes due to blockage of their arteries. Reduced blood flow coupled with elevated blood sugar levels provides an ideal environment for the growth and proliferation of bacteria, which leads to the development of serious infection.
Though the changes and effects caused by vasculopathy in a diabetic patient are not reversible, doctors can help these patients heal their non-healing wounds. The first line of treatment is oral medicine, which helps increase blood flow. In an advanced stage of the disease, blocked arteries are opened either by angioplasty with the balloon (balloon angioplasty) or by stenting the vessel. Even though vessels thus opened tend to occlude in the course of time, increased blood flow from these salvage procedures helps immensely in the healing of non-healing wounds.
Yes, diabetic foot infections can be prevented to a large extent. Regular and proper care of both feet, along with 3 monthly foot check-ups by an expert plastic surgeon,, are the best ways to avoid/delay the occurrence of diabetic foot infection. Whenever suggested by a plastic surgeon, the use of customized protective footwear and the latest internal offloading surgery (performed by a trained and experienced plastic surgeon) are the most appropriate attempts to save the digits and limbs of a diabetic patient.
Plastic surgery is extremely beneficial and is advocated at all stages of diabetic foot infection. Starting from the very early stage of callus formation to the advanced stages of gangrene of the foot, the plastic surgeon plays the most important role by doing debridement (removal) of affected tissues, proper management of the wound along with daily dressings, preparation of the wound, and final coverage of the wound by one of the reconstructive plastic surgery techniques like skin grafting and flaps. Surgery like amputation also carries great significance.
A properly reconstructed amputation stump by a plastic surgeon makes the fitting of a prosthesis easy and effective. Ill-fitting prostheses or improper amputation stumps lead to non-healing ulcers, infections, or revision surgery. The latest plastic surgical technique of internal offloading is a boon for patients with diabetic foot. This internal offloading surgery is the best available tool to salvage the toes and foot and to heal resistant ulcers for a very long period of time.
Before understanding the concept of internal offloading, one needs to understand the mechanism of ulcer development in a diabetic patient. Diabetic patients develop alterations in the molecular structure of their collagen and elastin fibers.
These fibres though very tiny and microscopic structures, are the important building blocks of the fascia, ligaments, and tendons of the foot. Alteration in the elastin and collagen fibers causes a minor yet definite abnormality in the fascia, ligaments, and tendons of the foot.
Gradually, this minor abnormality magnifies and results in an obvious (yet not apparent) deformity of digits, forefoot or hindfoot, and tendons. This leads to abnormal amounts of pressure at some sites in the sole, which in turn is responsible for ulcer development at the corresponding site in the foot. If left untreated, the majority of these ulcers get deepened, involve underlying tendons, bones, and joints, and lead to amputation of the digit or foot. If the deformity responsible for foot ulcer development is addressed early, not only does the ulcer heal, but it does not reoccur most of the time.
Thus, the patient’s ulcer is cured, and at the same time, his/her digit and limb are saved. Internal offloading surgery is the name given to such miraculous plastic surgery aimed at healing the diabetic foot ulcer as well as preventing its recurrence.
Cutis Hospital is conveniently located in Ghatlodia, Ahmedabad, making it easily accessible via multiple modes of transportation. Below are the various ways you can reach our facility:
Sardar Vallabhbhai Patel International Airport: Located approximately 12.7 km from Cutis Hospital, offering convenient access for patients traveling from outside the city.
Chandlodiya Railway Station: Approximately 2.4 km from Cutis Hospital.
Ahmedabad Railway Station: Around 11 km from our center.
GSRTC:
Ahmedabad Central Bus Station (GSRTC): About 10.3 km from the hospital.
AMTS:
Bhuyangdev Cross Road Bus Stop: Just 500 meters from Cutis Hospital.
BRTS:
Bhuyangdev BRTS Bus Stop: Only 170 meters from our center.
We provide effective surgical and non-surgical treatments for all parts of the body. At Cutis Hospital, our cosmetic and plastic surgery team is committed to giving patients safe and high-quality care.